Patients with ITP are facing significant challenges
In a study, patients living with ITP reported significantly worse health-related quality of life (HRQOL) compared with the general US population. Their HRQOL was also lower than that of patients living with cancer and other serious chronic conditions.1*
*The study used the Short-Form 36 questionnaire to evaluate the HRQOL of 73 adult ITP patients compared with that of the general US population and of patients with 6 other relatively common chronic disorders.1
ITP can impact patient quality of life in multiple ways, including:
The true ITP impact: See how ITP affects Holly's life


Fatigue is common and often severe in patients with ITP2
“Fatigue is one of the horrible issues for ITP. I'd say I'm mostly at 75 to 60 percent energy on normal days.”
Kyle, real patient living with ITP

In the Immune Thrombocytopenia World Impact Survey (I-WISh)* of 1507 patients and 472 physicians, patients rated functional, psychological, and emotional aspects of their condition. In I-WISh2:

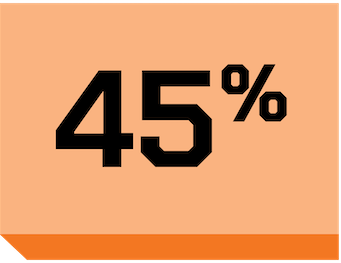
of patients reported fatigue at diagnosis (n=870/1507), and

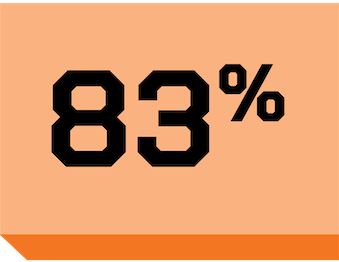
of those patients rated fatigue as severe (n=637/870)

In a separate study, severe fatigue was prevalent in approximately 47% of patients with low disease activity, and fatigue persisted even after platelet counts increased4†
*I-WISh was an online, cross-sectional survey of patients with ITP and hematologists or hemato-oncologists who treat patients with ITP in 13 countries. The patient questionnaire collected information on demographics and diagnosis, symptoms of ITP, health-related quality of life (HRQOL) and emotion associated with ITP, impact of ITP on work, finances, and support, treatment received, and patient and physician relationship. The physician survey comprised 6 sections that collected information on demographics, diagnosis of ITP and patient caseload, symptoms of ITP, impact of ITP on aspects of patients’ physical, emotional, HRQOL, social health, treatment patterns, and patient and physician relationship. There were 2 questions about the emotional impact of ITP and the responses were based on a 7-point Likert scale (1 = never, 7 = a great deal). There was 1 additional question on the need for professional support.5
†A cross-sectional study that included 59 adult patients with chronic ITP. Univariable linear regression, adjusted for confounders, was used to analyze relationships between disease activity, disease-specific factors, and transdiagnostic factors with fatigue.5
Ongoing studies are evaluating the role of inflammation that may contribute to fatigue in ITP4,6
But HCPs may not perceive patients’ fatigue at the same levels2
Of the HCPs surveyed in I-WISh2:
-03%201.png 200w)
reported hearing about fatigue at diagnosis (n=472) and rated
-04%201.png 200w)
of that fatigue as severe (n=465)

Heavy menstrual bleeding can have a major negative impact on patient QOL2
Of the 975 female patients interviewed in the I-WISh survey2:
reported heavy menstrual bleeding at diagnosis (n=439/975), and
of those said it was one of their most severe symptoms (n=364/439)
In the same survey, 78% of physicians (n=368/472) identified heavy menstrual bleeding as 1 of 3 signs or symptoms that have the largest impact on patient QOL2

TEs are more common among patients with ITP3
Patients with ITP face up to a
~2X higher risk of TEs
compared to the general population3*
Risk factors for TEs in ITP6,7
- Increased levels of immature hyperactive platelets
- Presence of prothromboembolic microparticles
- Endothelial activation
- Previous thromboembolism
- Age >60 years
- Cardiovascular (CV) risk factors
- Positive antiphospholipid antibodies (aPL)
- Antinuclear antibodies
- Surgery, immobilization
- Corticosteroids
- IVIg
- Splenectomy
- TPO-RAs
*Data from a retrospective cohort study of 1140 patients with ITP and 5657 patients without ITP. Adjusted risk ratio of 1.7 in venous thrombosis, 1.2 in central nervous system (CNS) arterial TEs, and 1.5 in non-CNS arterial TEs. Adjusted for smoking, arterial events, hyperlipidemia, hypertension, diabetes, cardiac arrhythmia, cerebral infarction due to occlusion/stenosis/embolism/thrombosis, cerebrovascular stenosis or occlusion, and related syndromes without infarction.3
IVIg, intravenous immunoglobulin; TPO-RA, thrombopoietin-receptor agonist.
Next: Mechanism of disease
Take an in-depth look at the immune pathways that drive ITP.
1. McMillan R, Bussel JB, George JN, Lalla D, Nichol JL. Self-reported health-related quality of life in adults with chronic immune thrombocytopenic purpura. Am J Hematol. 2008;83(2):150-154. 2. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (iWISh): patient and physician perceptions of diagnosis, signs and symptoms, and treatment. Am J Hematol. 2021;96(2):188-198. 3. Kuter DJ, Gouia I, Cordoba M, et al. Clinical burden of illness in patients with persistent or chronic primary immune thrombocytopenia treated with advanced therapies in the United States. Poster presented at: American Society of Hematology Annual Meeting & Exposition; December 7-10, 2024; San Diego, CA. 4. van Dijk WEM, Nap-van der Vlist MM, Knoop H, Schutgens REG. Possible targets to reduce fatigue in chronic immune thrombocytopenia patients - an explorative study. TH Open. 2022;6(4):e387-e395. 5. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (I-WISh): impact of ITP on health-related quality of life. Am J Hematol. 2021;96(2):199-207. 6. Hill QA, Newland AC. Fatigue in immune thrombocytopenia. Br J Haematol. 2015;170(2):141-149. 7. Saldanha A, Colella MP, Villaça PR, Thachil J, Orsi FA. The immune thrombocytopenia paradox: should we be concerned about thrombosis in ITP? Thromb Res. 2024;241:109109.

