ITP is characterized by symptoms such as low platelet counts, bleeding, and bruising1
ITP is an acquired autoimmune disorder characterized by low platelet counts that result from both increased platelet destruction and/or decreased platelet production.2-4
The time since diagnosis helps classify ITP as newly diagnosed, persistent, or chronic.5

Multiple symptoms of ITP are related to bleeding5-8:

Petechiae and purpura, typically in lower extremities
%201.png)
Bleeding blisters and epistaxis

Organ bleeding
(eg, menorrhagia)

Intracranial
hemorrhage
Severe bleeding occurs in 7% to 10% of adult patients and typically correlates with lower platelet counts.6,9*
*
As seen in a cross-sectional study of 302 French patients, as well as in a systematic review of 147 clinical studies of adults and children with primary ITP.6,9
While platelet counts below 100,000/μL can indicate ITP, the lack of a specific diagnostic test means other potential causes of thrombocytopenia must be ruled out.2,5
It is also important to determine if ITP is primary or secondary to another condition. There are multiple causes of secondary ITP, including chronic lymphocytic leukemia (CLL), Helicobacter pylori infection, and COVID-19 infection.5
ITP can occur in people of all ages. The incidence of ITP ranges from 2 to 4 cases per 100,000 person years in adults and children.2,11
The prevalence of ITP is estimated to be 58 per 100,000 adults and between 4.1 and 9.3 per 100,000 children (ages 1 to 18 years).12,13
The pathophysiology of ITP is complex and not fully understood2,14
In ITP, autoreactive B cells produce autoantibodies that target platelets for destruction by macrophages and impair megakaryocyte maturation, which then inhibits platelet production. Autoantibodies may also destroy platelets through other mechanisms. Cytotoxic T cells can also directly destroy or inhibit the production of platelets.2
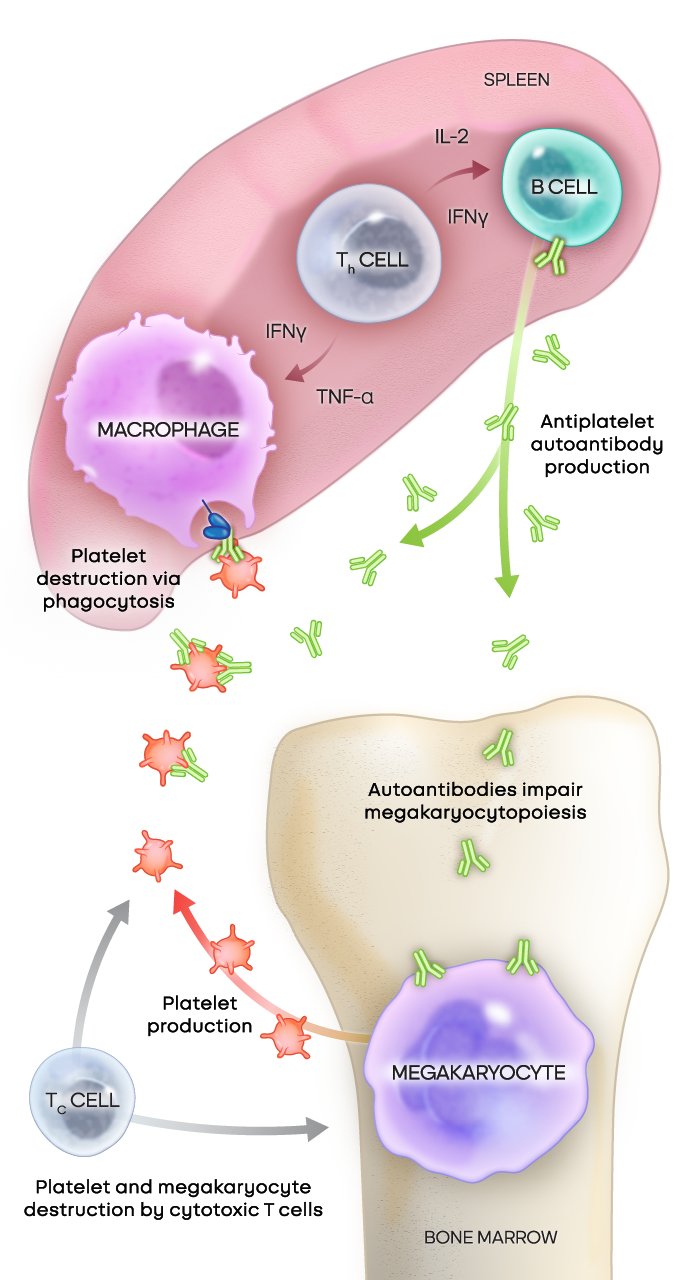
Adapted from Kashiwagi H, et al. Int J Hematol. 2013;98(1):24-33. © Japanese Society of Hematology (JSH)
Bruton’s tyrosine kinase (BTK) drives key processes in B cells and macrophages15,16
B cells are critical to autoantibody production and macrophages are critical to phagocytosis. Both of these processes are regulated by BTK.
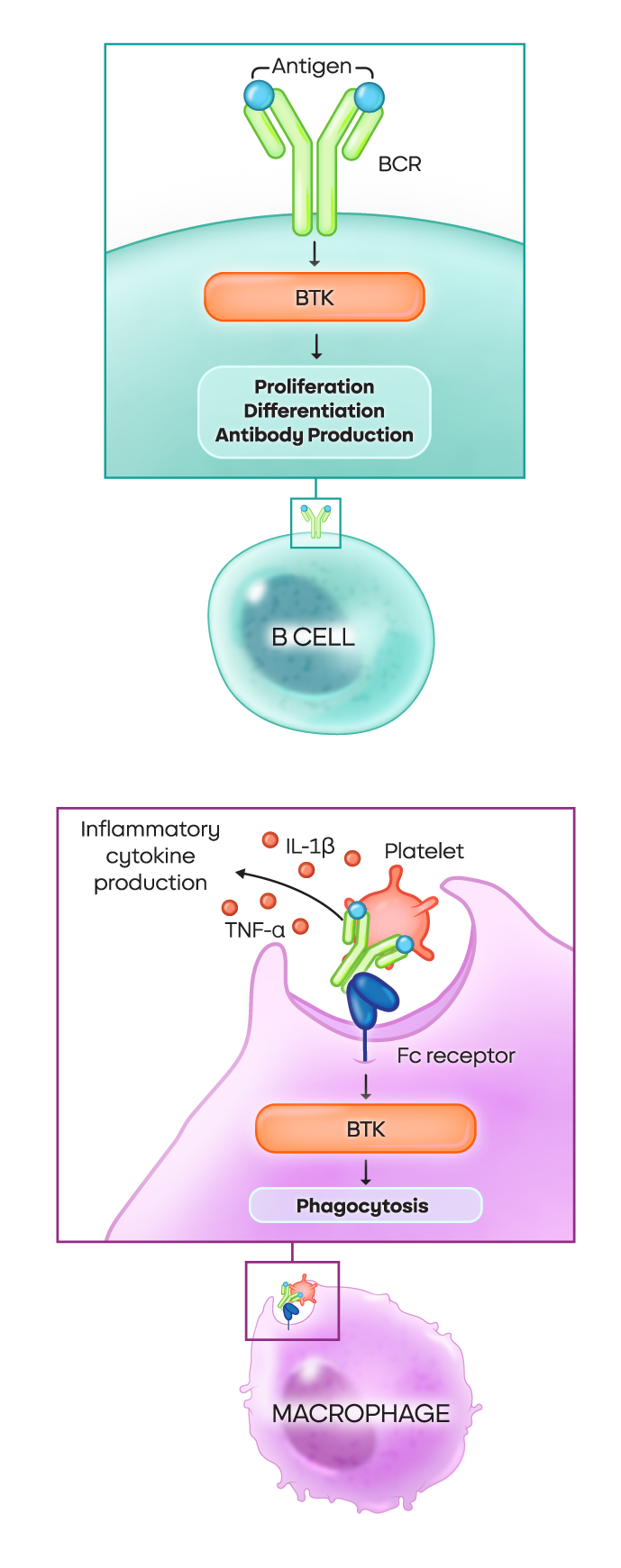
- In B cells: The BTK pathway is crucial for proliferation, differentiation, and autoantibody production
- In macrophages: Various signaling pathways dependent on BTK drive phagocytosis, degranulation, and the production of inflammatory cytokines
BTK is also a critical driver of inflammation16
BTK plays a critical role in the production or activation of these inflammatory markers:
• TNF-α
• IL-6
• NLRP3 inflammasome
• IFN-γ
Next: ITP is about more than platelets
Learn how ITP symptoms like fatigue and cognitive impairment impact patients’ quality of life.
1. Rovó A, Cantoni N, Samii K, et al. Real-world impact of primary immune thrombocytopenia and treatment with thrombopoietin receptor agonists on quality of life based on patient-reported experience: results from a questionnaire conducted in Switzerland, Austria, and Belgium. PLoS One. 2022;17(4):e0267342. 2. Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945-955. 3. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (I-WISh): impact of ITP on health-related quality of life. Am J Hematol. 2021;96(2):199-207. 4. Mitchell E, Frith J, Newton J. Fatigue and cognitive impairment in immune thrombocytopenic purpura remain stable over time: short report from a longitudinal study. Br J Haematol. 2019;186(5):777-781. 5. Arnold DM, Cuker A, et al. Immune thrombocytopenia (ITP) in adults: clinical manifestations and diagnosis. UptoDate. Updated July 26, 2023. Accessed September 29, 2023. https://www.uptodate.com/contents/immune-thrombocytopenia-itp-in-adults-clinical-manifestations-and-diagnosis 6. Piel-Julian M-L, Mahévas M, Germain J, et al. Risk factors for bleeding, including platelet count threshold, in newly diagnosed immune thrombocytopenia adults. J Thromb Haemost. 2018;16(9):1830-1842. 7. Cooper N, Morrison MA, Vladescu C, et al. Identification of occult cerebral microbleeds in adults with immune thrombocytopenia. Blood. 2020;136(25):2875-2880. 8. van Dijk WEM, Nap-van der Vlist MM, Knoop H, Schutgens REG. Possible targets to reduce fatigue in chronic immune thrombocytopenia patients - an explorative study. TH Open. 2022;6(4):e387-e395. 9. Neunert C, Noroozi N, Norman G, et al. Severe bleeding events in adults and children with primary immune thrombocytopenia: a systematic review. J Thromb Haemost. 2015;13(3):457-464. 10. Arnold DM, Cuker A, et al. Diagnostic approach to thrombocytopenia in adults. UptoDate. Updated August 30, 2023. Accessed September 29, 2023. https://www.uptodate.com/contents/diagnostic-approach-to-thrombocytopenia-in-adults 11. Schoonen WM, Kucera G, Coalson J, et al. Epidemiology of immune thrombocytopenic purpura in the General Practice Research Database. Br J Haematol. 2009;145(2):235-244. 12. Sanofi Genzyme. Data on file. 13. Segal JB, Powe JB. Prevalence of immune thrombocytopenia: analyses of administrative data. J Thromb Haemost. 2006;4(11):2377-2383. 14. Kashiwagi H, Tomiyama Y. Pathophysiology and management of primary immune thrombocytopenia. Int J Hematol. 2013;98(1):24-33. doi:10.1007/s12185-013-1370-4 15. Zhu S, Gokhale S, Jung J, et al. Multifaceted immunomodulatory effects of the BTK inhibitors ibrutinib and acalabrutinib on different immune cell subsets - beyond B lymphocytes. Front Cell Dev Biol. 2021; 9:727531. 16. Neys SFH, Hendriks RW, Corneth OBJ. Targeting Bruton's tyrosine kinase in inflammatory and autoimmune pathologies. Front Cell Dev Biol. 2021;9:668131.